IgGFc-binding protein and MUC2 mucin produced by colonic goblet-like cells spatially interact non-covalently and regulate wound healing.
June 25, 2023

The mucus protective layer in the colon serves as the first line of innate host defense against potential pathogens and also provides a niche and nutrient source for indigenous microbiota. In a recent study by a Snyder Institute research team (led by Dr. Kris Chadee; first author Hayley Gorman) published in Frontiers in Immunology, researchers aimed to understand how two important components of mucus, called MUC2 mucin and FCGBP protein produced by goblet cells, interacted together to strengthen the mucus layer to maintain epithelial barrier function.
IgGFc-binding protein and MUC2 mucin produced by colonic goblet-like cells spatially interact non-covalently and regulate wound healing.
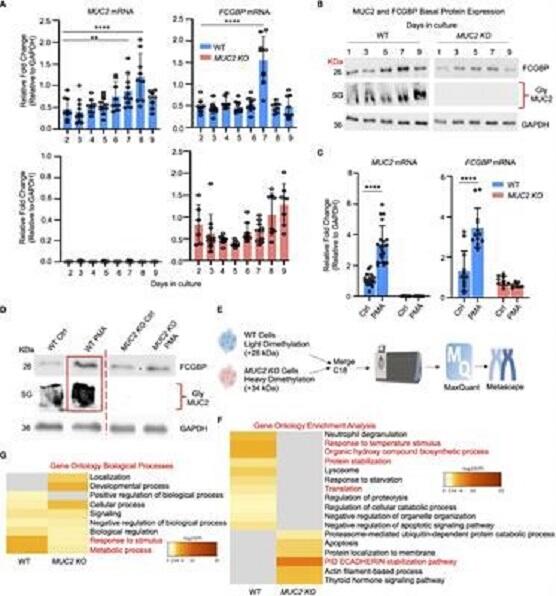
Results of the study revealed that MUC2 and FCGBP were colocalized in mucus granules and were secreted together to form the mucus barrier. Biochemical analysis revealed that MUC2 and FCGBP interacted via N-linked glycans, whereas FCGBP interacted covalently with other mucus associated proteins. Importantly, the research team identified a cytoplasmic pool of FCGBP not bound to MUC2 mucin that enhanced wound healing by increasing the production of growth factors, cell migration and proliferation.
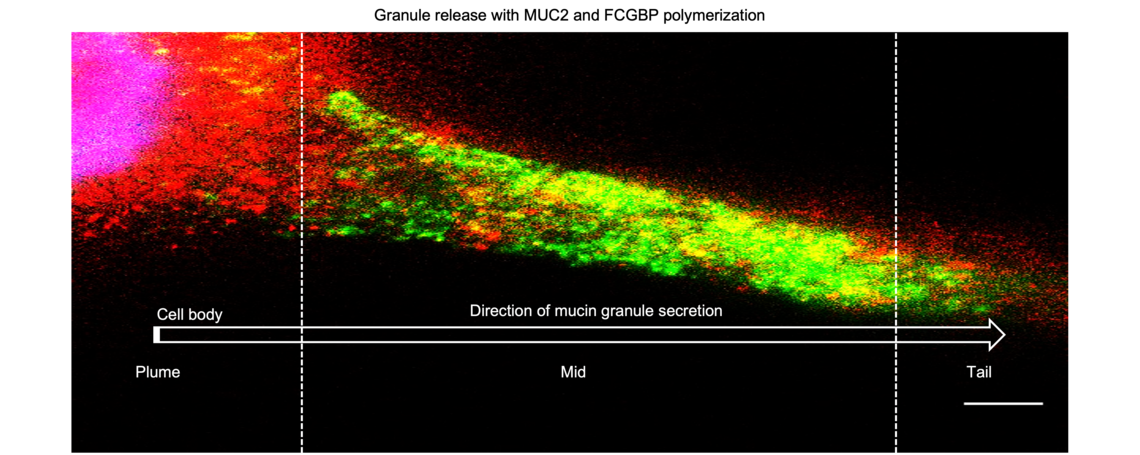
Granule release with MUC2 adn FCGBP polymerization
Overall, this study highlights the complex interactions between MUC2 mucin, FCGBP protein, and other components of the mucus layer in epithelial barrier function. Understanding these interactions may provide insights into potential therapies to fortify and maintain a healthy gut barrier and in promoting wound healing in inflammatory bowel diseases and infectious colitis.